end stage renal disease after kidney transplant
End-stage Renal Disease
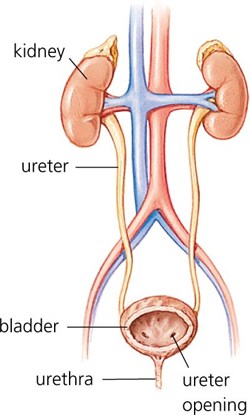
The kidneys are two bean shaped organs whose function is essential to life. The kidneys are located on either side of the spine behind the abdominal organs and below the rib cage. The kidneys perform several major functions:
- Filtration of the blood to remove waste products from normal body functions, passing the waste from the body as urine, and returning water and chemicals back to the body as necessary.
- Regulation of the blood pressure by releasing several hormones.
- Stimulation of production of red blood cells by releasing the hormone erythropoietin.
The kidneys produce urine, which is then carried to the bladder by the ureters. The bladder serves as a storehouse for the urine. When the body senses that the bladder is full, the urine is excreted from the bladder through the urethra.
Chronic Kidney Disease
In chronic kidney disease, also known as CKD, there is an accumulation of toxic waste products in the body resulting in permanent damage to the kidneys. While the kidneys may work well enough for a person to live, the condition is irreversible and often worsens over time until the kidneys fail known as end-stage renal disease (ESRD) .
Causes
Diabetes and high blood pressure are the leading causes of chronic kidney disease and kidney failure. The disease can also be caused by a physical injury to the kidney or by other diseases. When the kidneys are damaged, they do not effectively remove wastes and extra water from the blood.
Symptoms
In its early stages, CKD is often silent producing few if any symptoms. CKD often develops so slowly, in fact, that many people are unaware of it until the disease is very advanced or must be rushed to the hospital for life-saving dialysis. CKD runs in families. There is an increased risk of developing the disease if a first-degree relative (mother, father, sister, or brother) has kidney failure.
Risks of Developing CKD
- Diabetes
- High Blood pressure
- Kidney failure in a first-degree relative
Some racial groups are at increased risk for CKD
- African Americans are nearly four times as likely to develop kidney failure as white Americans.
- American Indians have nearly three times the risk compared to whites.
- Hispanic Americans have nearly twice the risk of non-Hispanic whites.
If a person has one of these risk factor, they should be screened for kidney disease which is done through simple blood and urine tests.
Diagnosis
Since early CKD has no symptoms, the diagnosis is made using standard medical tests.
- Blood Pressure: High blood pressure can lead to kidney damage, and it can also be a sign that kidney damage has already occurred. If blood pressure is high, controlling it is essential to ensure the kidneys remain healthy.
- Blood Test: The glomerular filtration rate (GFR) measures how efficiently the kidneys are filtering waste from the blood. The new method of calculating GFR requires only a measurement of the creatinine (kree-AT-ih-nin) in a blood sample. Creatinine is a waste product in the blood created by the normal breakdown of muscle cells during activity. When kidneys are not working well, creatinine builds up in the blood.
- Urine Test: Measuring the amount of a protein called albumin in the urine can show a kidney problem. A large amount of protein in the urine is known as proteinuria and is a sign of kidney damage. A dipstick in a sample of your urine is used for this test. The color of the dipstick indicates the level of protein.
A test that can show smaller amounts of protein or albumin in the urine is called a microalbumin test and also uses a dipstick in the urine. Your doctor may also do a calculation of the protein-to-creatinine or albumin-to-creatinine ratio. Healthy kidneys move creatinine from the blood into the urine. A ratio greater than 30 milligrams of albumin per 1 gram of creatinine indicates that the kidneys are leaking helpful substances from the blood and failing to filter out harmful substances. This test should be used in people at high risk, especially those with diabetes.
If your first laboratory test shows high levels of protein, another test should be done 1 to 2 weeks later. If the second test also shows high levels of protein, you have persistent protein in the urine (proteinuria) and should have additional tests to test your kidney function.
A 24-hour urine collection is no longer necessary. Small samples of urine and blood, which can easily be taken in the doctor's office, are all the new methods require.
A 24-hour urine collection is no longer necessary. Small samples of urine and blood, which can easily be taken in the doctor's office, are all the new methods require.
Several organizations offer free screenings for kidney disease. You may be able to have your kidney function measured at a local health fair. The National Kidney Foundation's KEEP (Kidney Early Evaluation Program) initiative offers blood and urine testing, on-site consultation with a physician, and referral and followup services for people whose test results are outside the normal range.
The American Kidney Fund's MIKE (Minority Intervention and Kidney Education) Program offers educational sessions and medical screenings. The American Association of Kidney Patients' Finding Your Strength program offers education about your kidneys, tests to expect, and ways to stay healthy with CKD. Contact information for these and other organizations appears in the For More Information section at the end of this fact sheet.
What can I do to slow down or avoid kidney failure?
Learning about reduced kidney function allows you to take steps to keep your kidneys healthy as long as possible. You can control many of the things that can make CKD worse and may lead to kidney failure.
- If you have diabetes, control your blood glucose, also called blood sugar. Studies show that keeping tight control of blood glucose can delay or prevent kidney failure.
- If you have high blood pressure, keep your blood pressure below 140/90 mm Hg.
- If you have high blood pressure with CKD, keep your blood pressure below 130/80 mm Hg. Blood pressure medicines called ACE (angiotensin-converting enzyme) inhibitors and ARBs (angiotensin receptor blockers) protect the kidneys better than other medicines. You may need a combination of two or more drugs to keep your blood pressure below 130/80. In many cases, a medicine that lowers blood pressure by increasing urination, called a diuretic, should also be part of the plan.
- If you have CKD, don't eat too much protein. Protein breaks down into the waste products the kidneys must excrete. Reducing those waste products by eating less protein means the kidneys don't have to work so hard. But eating too little protein can lead to poor nutrition. Work with a dietitian to make sure you get the right amounts of protein and other nutrients.
What can I do to avoid the complications of CKD?
CKD can lead to many other health problems well before kidney failure occurs.
- Anemia. Anemia develops when the kidneys fail to produce enough erythropoietin, or EPO, the hormone that directs the bones to make red blood cells. Anemia can cause heart problems.
- Bone problems. Healthy kidneys help keep your bones strong by balancing the levels of calcium and phosphorus in the blood. CKD can lead to bone problems by throwing those minerals out of balance.
- Acidosis. The kidneys also maintain the acid/base balance in the blood. Kidney problems may lead to acidosis, a condition in which the blood is too acidic. Acidosis can disrupt body functions.
- Cardiovascular disease (CVD). Patients with CKD are more likely to die from a heart attack or stroke than from kidney failure. Even a small loss of kidney function can double a person's risk of developing CVD.
If you have CKD, you will need to have regular checkups to monitor blood levels of creatinine, urea nitrogen, potassium, phosphorus, parathyroid hormone, hemoglobin, and cholesterol. If your blood tests show abnormal levels of any of these substances several times, your doctor will prescribe medicines. For example, if you have anemia indicated by low levels of hemoglobin on repeated tests, your doctor can prescribe a synthetic form of EPO (erythropoietin) to help your body make more red blood cells.
End Stage Renal Disease (Kidney Failure)
Chronic kidney disease may eventually result in complete kidney failure. This is the last stage of CKD (Stage 5), also referred to as end-stage renal disease (ESRD). When the kidneys totally fail, either dialysis or a kidney transplant is required.
Common Causes of End-Stage Renal Disease
- Diabetes mellitus
- High blood pressure
- Glomerulonephritis
- Polycystic Kidney Disease
- Severe anatomical problems of the urinary tract
Dialysis
- Hemodialysis, a mechanical process of cleaning the blood of waste products
- Peritoneal dialysis, in which waste products are removed by passing chemical solutions through the abdominal cavity
Kidney Transplantation
Dialysis does not cure end-stage renal disease. A transplant offers the closest thing to a normal life because the transplanted kidney can replace the failed kidneys. However, a kidney transplant also involves a life-long dependence on drugs to keep the new kidney healthy. Some of these drugs can have severe side effects.
Some kidney patients consider a transplant after beginning dialysis; others before starting dialysis. Dialysis patients who also have severe medical problems such as cancer or active infections may not be suitable candidates for a kidney transplant.
A Growing Problem
CKD is a growing problem in the United States of which kidney failure is only one piece. Experts estimate that 20 million Americans have significantly reduced kidney function; even a small loss of kidney function can double a person's risk of developing cardiovascular disease. Many of these people will experience heart attacks or strokes before they become aware of their kidney disease. So identifying and treating CKD early can help prevent heart problems as well as postpone kidney failure.
Source : https://transplantsurgery.ucsf.edu/


Leave a Comment