Computed tomography (CT)
Overview
The patient is lying on a table and it will move through a ring. This ring contains an X-ray tube and a set of detectors. With axial CT, it is the X-ray beam that rotates around the patient and, during the examination, the patient should lie still on the table. The X-ray detectors are the equivalent of the film: they are the ones that will collect the characteristics of the X-ray beams that have passed through the patient's body. This information is analyzed by a computer and will make it possible to create an image.Image formation
at each rotation and for each degree traversed by the tube, the detectors receive information on the quantity of x-rays passing through the patient. The multiple digital data received by the computer make it possible to construct images corresponding to successive sections of the region studied. These successive sections correspond to what is scientifically called axial sections (fig. 1).
Axial (fig. 1)
Note: It is the slow movement (the advance) of the table through the ring (in which the X-ray tube rotates) which allows the continuous / successive acquisition of the axial sections of an entire region.
With the scanner, there is no longer any superposition of the different organs on the same image as with a chest X-ray for example. On a CT scan, the organs can be studied individually (fig. 2). The gray range of the images obtained with the CT scan makes it possible to detect differences between the tissues: bone (white), aerated pulmonary parenchyma (black) and muscle (gray). The minimum size for detecting lesions (resolution) is also greatly improved with the scanner. These facts explain the superiority of detection of pulmonary lesions of the scanner (computed tomography) on the standard radiography of the thorax.
Axial - computed tomography (CT) of the thorax - mediastinal window
(fig. 2)
The images provided by the scanner are in the axial plane. Thanks to the raw data stored on the hard drives of the calculator, computer programs make it possible to reconstruct images in the sagittal or coronal plane (fig. 3). The finer the native axial sections, the better the resolution of the sagittal or coronal reconstructions.

Coronal reconstruction of the body after a CT scan (fig. 3)
Images 4 and 5 are from a CT scan of a leg. Images 6 and 7 are from a CT scan of the chest.
By manipulating the digital image data, multiple and new information can be collected and we obtain a different vision (and therefore information) of the same organ. Here are two axial CT sections of a leg: the first time seen from the "bone" angle (fig.4) then the second time from the "soft tissue" angle (fig.5). These digital manipulations make it possible to simultaneously acquire information on the bone structures and on the soft parts of the leg.

CT scan of the leg - axial section ("bone window") (fig.4)

CT scan of the leg-axial ("soft tissue window") (fig.5)
Here are two CT scans of the thorax: the first time seen from the "mediastinal" angle (fig.6) then the second time from the "pulmonary parenchyma" angle (fig.7). These digital manipulations allow us to simultaneously have information on the mediastinal structures (lymph nodes, vessels, etc.) and the state of the pulmonary parenchyma (emphysema bubbles, tumor, etc.).

Thoracic CT scan - soft tissue window. (Fig.6)

Thoracic computed tomography - parenchymal window (fig. 7).
Diagnostic information
The information is taken from the differences in X-ray absorption between normal tissue and pathological tissue. The greater the difference in absorption, the more easily the lesion is detectable. Conversely, if the pathological tissue has radiological properties close to that of healthy tissue, it can be difficult to identify.
The intravenous contrast injection clearly provides additional information. It provides diagnostic information:
• anatomically (location of vessels in the thorax versus ganglion)
• on the angiodynamic behavior of the lesions
• the structure of the lesions.
This information can help formulate a hypothesis on the nature of the lesion observed (= characterization).
The CT aspect of a tissue is described in terms of its density relative to the adjacent structures.
A lesion can be described as:
• hyper-dense (= light color)
• hypo-dense (= dark color) or iso-dense (= identical color) compared to the surrounding fabric.
In general, an iso-dense lesion is only discovered by the anatomical anomalies which arise from its expansion (compression of vessels, deformation of the outline of the organs).
The density of a lesion may or may not vary after intravenous contrast injection. During the examination, the appearance of the lesion can vary over time and it is this dynamic aspect that allows to characterize lesions such as hepatic hemangioma
When the lesion is cystic, its density is between 0 and 10 Hounsfield units. The density of fresh blood is around 50-60 Hounsfield units. Note that the density of a hematoma gradually decreases over the course of one to two weeks. For grease, the density is between -40 and -140 Hounsfield units.

Computed tomography of the abdomen: bulky hyperdense post-operative collection (density of 66 Hounsfield U): hematoma.
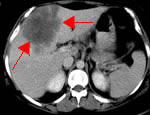
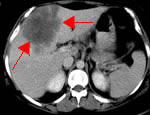
Computed tomography of the liver: large hypodense lesion (density of 35 Hounsfield U) of the liver: metastasis.
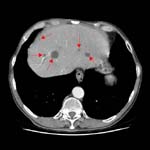
Computed tomography of the liver: multiple biliary cysts (density 8 Hounsfield U) in a patient with polycystic kidney disease.
Indications / limitations / performance of a computed tomography examination
For brain exploration, in regions where MRI is easily accessible, the scanner has fallen somewhat into disuse. Its indications today mainly concern patients who have had a head trauma or in whom one suspects an intracranial hemorrhage. This examination is also performed before a lumbar puncture to exclude intra cranial hypertension. Magnetic resonance imaging gives such luxury of details in the description of the anatomy, gray / white matter, cerebral nuclei that it has supplanted the scanner in the search for non-traumatic brain pathologies.
For the exploration of the thorax, the scanner remains today still the best radiological examination. It allows an excellent appreciation of the pulmonary parenchyma as well as the mediastinum. As the question has been asked many times, it is emphasized that the resolution of a scanner dedicated to the study of the thorax does not make it possible to detect a small breast cancer. (Bar point!)
For the exploration of the abdomen, the scanner remains one of the best radiological examinations today. It allows a good appreciation of all the “full” intra-abdominal organs. For a search for abscesses or inflammatory intestinal pathologies such as diverticulitis, the scanner is the modality of choice. The improved performance of scanners and software has enabled the emergence of new indications for computed tomography: virtual colonoscopy. This is a technique dedicated to the search for polyps or colonic tumors.
The cholangioCT technique allows the study of the intra- and extra-hepatic bile ducts. EnteroCT is dedicated to the study of the small intestine. These latter techniques are in competition with MRI.
Note that for technical reasons, an abdominal scanner cannot detect lumbar disc herniations even if the spine is part of the region examined. A herniated disc can only be demonstrated by a CT scan dedicated only to the lumbar spine.
The scanner remains the examination of choice in the evaluation of bone lesions such as fractures. However, it is supplanted by MRI in the search for diffuse metastatic bone infiltration, in the study of non-bone structures such as the intervertebral discs or the spinal cord, in the search for meniscal or ligamentary pathologies (knee for example ).
The scanner (angioCT) has become the routine examination in vascular pathologies such as the search for pulmonary embolism or aortic dissection.
The CT scan has little use in studying soft tissue except to look for calcifications in a tumor. It has been completely replaced by MRI in this area.
CT versus MRI
CT and MRI are two methods that use different techniques: X-rays for the first; magnetic fields for the second. Consequently, these methods do not "see" the same thing and, therefore, the information provided is different. These are also two methods which can be complementary.
Each of the two modalities has its strengths and weaknesses:
• MRI has a high contrast sensitivity (= possibility of distinguishing multiple categories of soft tissue) and it excels in the search for lesions of the musculoskeletal systems or the cerebral nervous system.
Note that MRI has a lower resolution than that of computed tomography.
• Axial computed tomography provides very high resolution images of the abdomen or thorax. Ease of installation of patients, good tolerance, speed of image acquisition are other qualities of the CT examination to be mentioned. Computed tomography also excels in finding fractures, calcium or blood in the tissues. It is for all these reasons that the cerebral scanner remains the king exam in traumatic lesions (subdural hematoma) or the search for hemorrhage.
note that computed tomography has a contrast resolution much lower than that of MRI.
Risks of a CT scan
The CT scan is an effective and proven test. Risks from X-rays, administration of contrast media, etc. are discussed on their own pages accessible via the drop-down menu under the heading "Risks"
Risk of hematoma at the injection site
For most CT scans, it is necessary to inject a small volume of contrast in a fairly short time. This is done by means of a pump and a catheter generally placed in a vein of the fold of the elbow. When the catheter is badly positioned in the vein or if there is a weakening of the venous walls, during the injection, under the effect of the pressure, the contrast agent can leave the vein, deposit in the soft tissues neighborhood and cause the formation of a hematoma. The doctor or technician in charge of the examination is present during this injection and can stop it at any time, so this complication is rare. In case of occurrence, local treatment is rarely necessary.
Bibliography
• Cohan RH, Dunnick NR, Leder RA, Baker ME. Extravasation of nonionic radiologic contrast media: efficacy of conservative treatment. Radiology. 1990 Jul; 176 (1): 65-7.
• Birnbaum BA, Nelson RC, Chezmar JL, Glick SN. Extravasation detection accessory: clinical evaluation in 500 patients. Radiology. 1999; 212: 431-438.
• Wang CL, Cohan RH, Ellis JH, Adusumilli S, Dunnick NR. Frequency, management, and outcome of extravasation of nonionic iodinated contrast medium in 69,657 intravenous injections. Radiology. 2007 Apr; 243 (1): 80-7.
Saving images
The images obtained during a CT scan are of the "digital" type. They can therefore be stored on media such as a CD or DVD. They can be fixed on "films" via a laser printer. CT scans can be archived in computer systems and medical information management (PACS, RIS).
A few words on the history of axial CT imaging (CT, CAT-scan)
1972 First scanner built (EMI Mark I head scanner)
Hounsfield GN computerized transverse axial scanning (tomography). Br J Radiol 1973; 46: 1016
1984 electron beam scanner (Imatron, Electron Beam Tomography (EBT))
1990 Appearance of the helical scanner
Kalender WA, Seissler W, Klotz E, Vock P Single-breath-hold technique, continuous transport, and continuous scanner rotation. Radiology 1989; 176: 181
1993 CT scanner 2 strips (Elscint)
1997 The new revolution: the 4-bar scanner with a rotation time of less than 1 second.
Klingenbeck-Regn K, Schaller S, Flohr T, Ohnesorge B, Kopp AF, Baum U Subsecond multi-slice computed tomography: basics and applications. Eur J Radiol. 1999 Aug; 31 (2): 110-24.
2000s CT scanner 8 strips
2003s CT scanner 16 strips
2005s CT scanner 64 strips + CT scan "dual source"
2007s CT scanner 256 strips


Leave a Comment